BACKGROUND
Cesarean section (CS) is a life-saving procedure for mother and newborn. However, too often c-section is not available, is provided without adequate quality, or is provided when not medically indicated - all dimensions that lead to maternal and newborn mortality and morbidity. We see an opportunity to nurture the field to identify and demonstrate feasibility of interventions to address challenges related to safe, timely, and appropriate cesarean section in low and middle income countries.
THE CHALLENGE
We invite proposals for interventions to address the following challenges related to the cesarean section:
- Increasing access to cesarean section where it is currently inadequate
- Increasing quality and safety of cesarean section to reduce iatrogenic harm to both mothers and newborns
- Reducing rates of non-medically indicated cesarean section.
Interventions addressing more than one challenge (e.g. quality and access) are encouraged. In some geographies all three of these challenges exist simultaneously, at different times for different populations; in other geographies only one or two of these challenges predominate. Applications should clearly state which of these three challenges is being targeted and provide clear rationale for why the intervention is likely to address the challenge. We are particularly interested in geographies with high fertility and weak health systems that will face challenges to ensure the provision of safe c-sections can keep pace with medical need, and we will thus consider applications proposing activities to be implemented in Sub-Saharan Africa or South Asia (India, Pakistan, Bangladesh).
Grant Funding Levels
We seek to make Seed Grants to generate proof of concept of novel interventions together with Validation Grants to generate further evidence of feasibility at a larger scale for existing interventions.
- Seed Grants of $100K for up to 24 months: These grants are intended to provide proof of concept of an intervention that is entirely novel at small scale (e.g., single facility or district). Applicants should conduct a literature review to verify that the proposed intervention has no documented evidence; documentation of the methods and outcomes of this review must be provided in the application. These grants should demonstrate the feasibility of a novel intervention and its impact on one or more of the c-section challenges identified in this call for applications.
- Validation Grants of $300K for up to 24 months: These grants are intended to demonstrate the feasibility of a single intervention or a combination of interventions at the scalable unit [1] of a health system. Validation grants must replicate, confirm or more rigorously test one intervention - or multiple interventions - that have previously demonstrated proof of concept at a smaller scale. Given the complexity of the problem, we acknowledge that multi-component interventions are required, and we eoncourage applications exploring these.
What We Are Looking For:
All applications should:
- Focus on health service or delivery innovation. This call for applications excludes development of new medical devices and non-interventional analysis of data
- Describe how the intervention will be tailored to the epidemiology and health system where it will be implemented
- Ensure that women and newborns receive care that respects and preserves their dignity, including informed consent[2]
- Include participation from institutions based in South Asia and sub-Saharan Africa; applications led by institutions from these geographies are encouraged
- Propose interventions that align with the attributes of scalable health innovations[3]
- Report impact on c-section rates disaggregated by Robson classification[4], and safety with indicators such as case fatality rates and rates of post-operative complication
- Propose activities to be implemented in a country in Sub-Saharan Africa or South Asia (India, Pakistan, Bangladesh).
A few of the many options we will consider include (but are not limited to): clinical team huddles for improving quality of CS; interventions to improve immediate breastfeeding and bonding among mother-infant pairs after CS; interventions to improve communication between patient and care team; restructuring labor wards to facilitate latent phase labor management; adjustments to financial incentives related to CS; policy and liability reform.
We will not consider funding for approaches that have been widely used and evaluated in LMIC settings to scale up access to cesarean section (e.g., task shifting); activities to improve quality of care that already have extensive evidence of effectiveness; emergency transport interventions; mass media campaigns; or development of new tools for surgery, anesthesia, or patient monitoring.
Collaboration
This request for proposals seeks to create a consortium of individually funded projects that will benefit from sharing information between projects. We expect that such sharing will help to ensure that the goals of the innovative approaches in individual projects are ultimately integrated with each other, thereby increasing the chances that the programs will be greater than the sum of their parts. Furthermore, we expect that sharing experimental methods, data, and resources will ultimately improve the ability to compare and validate local research findings and to develop interventions and products. We expect to bring together all grantees after 18-24 months to share what they have learned in their work and to discuss how to accelerate progress with these lessons.
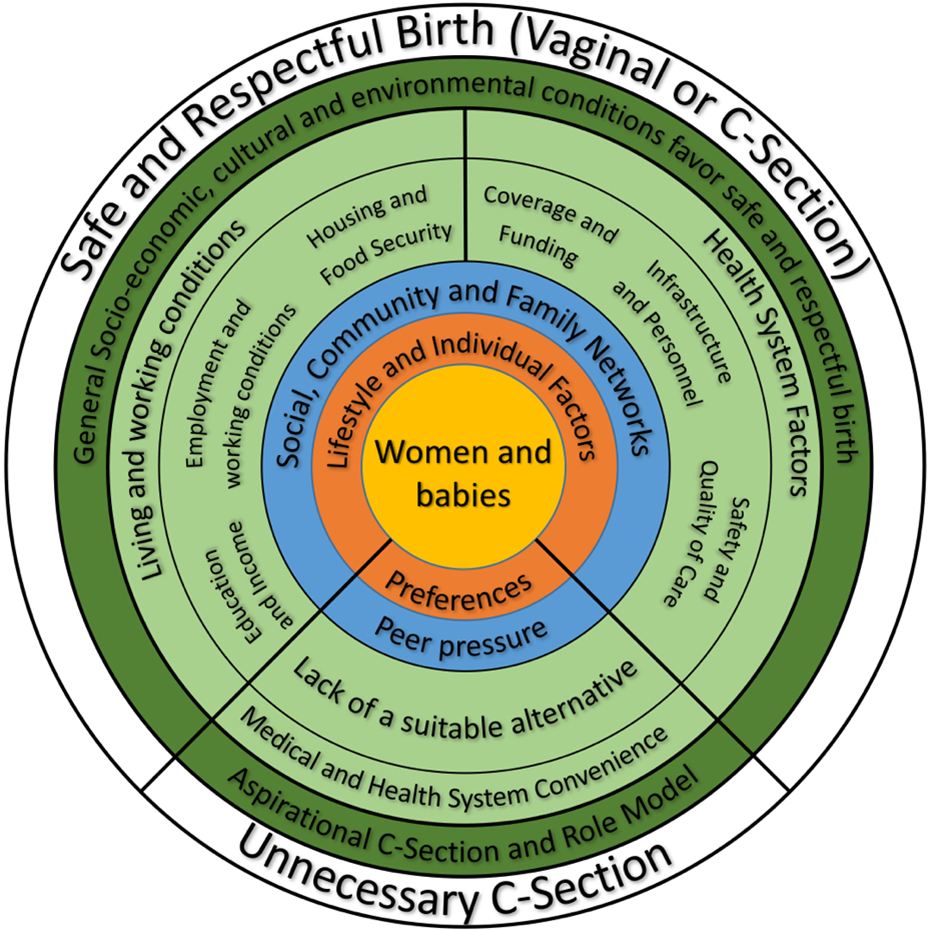
Figure 1. Framework for considering cesarean section
________________________________
[1]Barker P, Reid A, Schall M. A Framework for scaling up health interventions: lessons learned from large scale improvement initiatives in Africa. Implementation Science. 2016.
[2]WHO. Standards for Improving Quality of Maternal and Newborn Care in Health Facilities. 2016.
[3]Spicer et al. "Scaling-up is a craft not a science: Catalysing scale-up of health innovations…" Social Science and Medicine. 2014"
[4]WHO. Robson Classification: Implementation Manual. 2017
Opportunity Description
BACKGROUND
Cesarean section (CS) is a life-saving procedure for mother and newborn. However, too often c-section is not available, is provided without adequate quality, or is provided when not medically indicated - all dimensions that lead to maternal and newborn mortality and morbidity. We see an opportunity to nurture the field to identify and demonstrate feasibility of interventions to address challenges related to safe, timely, and appropriate cesarean section in low and middle income countries.
THE CHALLENGE
We invite proposals for interventions to address the following challenges related to the cesarean section:
- Increasing access to cesarean section where it is currently inadequate
- Increasing quality and safety of cesarean section to reduce iatrogenic harm to both mothers and newborns
- Reducing rates of non-medically indicated cesarean section.
Interventions addressing more than one challenge (e.g. quality and access) are encouraged. In some geographies all three of these challenges exist simultaneously, at different times for different populations; in other geographies only one or two of these challenges predominate. Applications should clearly state which of these three challenges is being targeted and provide clear rationale for why the intervention is likely to address the challenge. We are particularly interested in geographies with high fertility and weak health systems that will face challenges to ensure the provision of safe c-sections can keep pace with medical need, and we will thus consider applications proposing activities to be implemented in Sub-Saharan Africa or South Asia (India, Pakistan, Bangladesh).
Grant Funding Levels
We seek to make Seed Grants to generate proof of concept of novel interventions together with Validation Grants to generate further evidence of feasibility at a larger scale for existing interventions.
- Seed Grants of $100K for up to 24 months: These grants are intended to provide proof of concept of an intervention that is entirely novel at small scale (e.g., single facility or district). Applicants should conduct a literature review to verify that the proposed intervention has no documented evidence; documentation of the methods and outcomes of this review must be provided in the application. These grants should demonstrate the feasibility of a novel intervention and its impact on one or more of the c-section challenges identified in this call for applications.
- Validation Grants of $300K for up to 24 months: These grants are intended to demonstrate the feasibility of a single intervention or a combination of interventions at the scalable unit1 of a health system. Validation grants must replicate, confirm or more rigorously test one intervention - or multiple interventions - that have previously demonstrated proof of concept at a smaller scale. Given the complexity of the problem, we acknowledge that multi-component interventions are required, and we eoncourage applications exploring these.
What We Are Looking For:
All applications should:
- Focus on health service or delivery innovation. This call for applications excludes development of new medical devices and non-interventional analysis of data
- Describe how the intervention will be tailored to the epidemiology and health system where it will be implemented
- Ensure that women and newborns receive care that respects and preserves their dignity, including informed consent2
- Include participation from institutions based in South Asia and sub-Saharan Africa; applications led by institutions from these geographies are encouraged
- Propose interventions that align with the attributes of scalable health innovations3
- Report impact on c-section rates disaggregated by Robson classification4, and safety with indicators such as case fatality rates and rates of post-operative complication
- Propose activities to be implemented in a country in Sub-Saharan Africa or South Asia (India, Pakistan, Bangladesh).
A few of the many options we will consider include (but are not limited to): clinical team huddles for improving quality of CS; interventions to improve immediate breastfeeding and bonding among mother-infant pairs after CS; interventions to improve communication between patient and care team; restructuring labor wards to facilitate latent phase labor management; adjustments to financial incentives related to CS; policy and liability reform.
We will not consider funding for approaches that have been widely used and evaluated in LMIC settings to scale up access to cesarean section (e.g., task shifting); activities to improve quality of care that already have extensive evidence of effectiveness; emergency transport interventions; mass media campaigns; or development of new tools for surgery, anesthesia, or patient monitoring.
Collaboration
This request for proposals seeks to create a consortium of individually funded projects that will benefit from sharing information between projects. We expect that such sharing will help to ensure that the goals of the innovative approaches in individual projects are ultimately integrated with each other, thereby increasing the chances that the programs will be greater than the sum of their parts. Furthermore, we expect that sharing experimental methods, data, and resources will ultimately improve the ability to compare and validate local research findings and to develop interventions and products. We expect to bring together all grantees after 18-24 months to share what they have learned in their work and to discuss how to accelerate progress with these lessons.

Figure 1. Framework for considering cesarean section
________________________________
1Barker P, Reid A, Schall M. A Framework for scaling up health interventions: lessons learned from large scale improvement initiatives in Africa. Implementation Science. 2016.
2WHO. Standards for Improving Quality of Maternal and Newborn Care in Health Facilities. 2016.
3Spicer et al. "Scaling-up is a craft not a science: Catalysing scale-up of health innovations…" Social Science and Medicine. 2014"
4WHO. Robson Classification: Implementation Manual. 2017